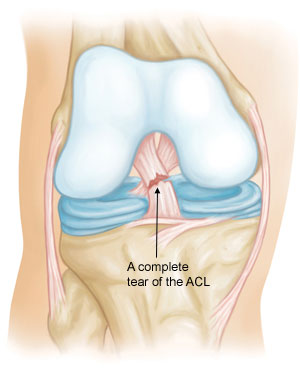
The desire to return to the pre-injury level of sports participation, particularly in sports involving cutting, pivoting, and jumping maneuvers, is a major reason for anterior cruciate ligament (ACL) reconstruction (Figure 1).
Studies indicate that after ACL reconstruction, on average 81% of people returned to any sport, 65% returned to their pre-injury level of sport and 55% returned to competitive level sports. The decision to allow an athlete to return to sport (RTS) after ACL reconstruction is based on the elapsed time after surgery (a surrogate for biological healing) and the patient’s functional capacity.
Incomplete rehabilitation and rushing back to sport can result in additional knee injuries and graft rupture. In addition to the physical recovery after an ACL reconstruction there are psychological factors that can affect an athletes readiness to return to sport as well.
A stable knee
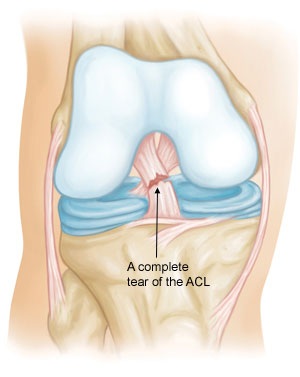
In order to participate in cutting and pivoting sports a stable knee is required, this usually means having an intact ACL. Damage to the ACL is a serious injury resulting in instability and poor function of the knee.
Although studies suggest that some individuals can return to sport without surgical reconstruction and adequate rehabilitation, the majority of patients continue to have knee instability requiring ACL reconstruction.
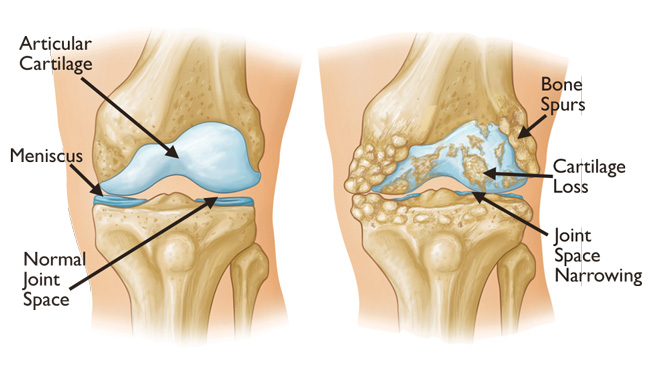
Sports participation with an unstable knee can lead to further injuries to the cartilage and the meniscus tissues (Figure 2), increasing the risk of future arthritis.
Treatment options
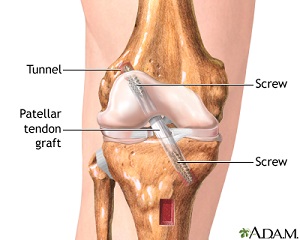
In order to reconstruct the torn ACL two common graft types are used – the patella tendon (Figure 3) or hamstrings (Figure 4).
Although no differences have been found in the rate of return to sport with the use of hamstring vs. patella tendon, several studies indicate the patella tendon graft results in better static knee stability and lower failure rate compared to hamstrings.
Use of a hamstring tendon graft can also result in decreased knee flexion strength. On the other hand the use of patella tendon graft can occasionally result in anterior knee pain and a slightly increased risk of ACL rupture in the opposite knee.
There is no perfect graft in ACL reconstruction and therefore the choice of graft needs to be individually tailored to the patient.

Return to sport
The decision regarding a return to sport is based on time to allow the graft to mature, functional status of the patient, and the psychological readiness to return to the sport and participate. Most evidence suggests waiting a minimum of 6-9 months before resuming pre-injury sports. Recent evidence reported a 50% reduction in risk of knee re-injuries (all injuries, not only ACL) for each month that a return to sport is delayed beyond 6 months up to 9 months. 3,6
Several objective tests are described for a return to sport. The maximum recommended differences between the operated and normal leg for return to sport clearance are between 10% and 15% in functional and strength testing. These tests include quadriceps and hamstring strength, single leg hop, triple hop and agility.6
Despite having an objectively stable knee after ACL reconstruction some patients do not return to sport due to fear of re-injury or the potential for their priorities to change. Some don’t consider the risk of re-injury acceptable and decide that they no longer wish to return to their particular sport. In the case of fear of re-injury it maybe useful to incorporate psychological techniques in the patient rehabilitation to maximise their ability to return to sport. 4
Summary
In summary there are several factors that contribute to a successful return to sport after ACL reconstruction. These include an objectively stable knee, adequate rehabilitation to regain strength and neuromuscular control, adequate time for graft maturity and psychological readiness. Expert support through out the process beginning with correct diagnosis, appropriate treatment and rehabilitation is paramount for a successful outcome.
References
1. Ardern, C. L., Taylor, N. F., Feller, J. A. & Webster, K. E. Return-to-sport outcomes at 2 to 7 years after anterior cruciate ligament reconstruction surgery. Am. J. Sports Med. 40, 41–8 (2012).
2. Ardern, C. L., Taylor, N. F., Feller, J. a & Webster, K. E. Fifty-five per cent return to competitive sport following anterior cruciate ligament reconstruction surgery: an updated systematic review and meta-analysis including aspects of physical functioning and contextual factors. Br. J. Sports Med. 48, 1543–52 (2014).
3. Grindem, H., Snyder-Mackler, L., Moksnes, H., Engebretsen, L. & Risberg, M. A. Simple decision rules can reduce reinjury risk by 84% after ACL reconstruction: the Delaware-Oslo ACL cohort study. Br. J. Sports Med. Epub ahead of print (2016). doi:10.1136/bjsports-2016-096031
4. Ardern, C. L. et al. The impact of psychological readiness to return to sport and recreational activities after anterior cruciate ligament reconstruction. Br. J. Sports Med. 48, 1613–1619 (2014).
5. Frobell, R. B., Roos, E. M., Roos, H. P., Ranstam, J. & Lohmander, L. S. A randomized trial of treatment for acute anterior cruciate ligament tears. N. Engl. J. Med. 363, 331–342 (2010).
6. Kyritsis, P., Bahr, R., Landreau, P., Miladi, R. & Witvrouw, E. Likelihood of ACL graft rupture: not meeting six clinical discharge criteria before return to sport is associated with a four times greater risk of rupture. Br. J. Sports Med. bjsports-2015-095908 (2016).
contact
Dr Shahrokhi is an orthopaedic sports specialist at sportsmed with a special interest in knee, hip and shoulder conditions. If you would like to make an appointment or enquiry with Dr Shahrokhi, contact 08 8362 7788 or email ortho@sportsmed.com.au.